
Anything in excess (including love & democracy) will lead to trouble. This is true of muscular contractions too. The muscle usually remains in a partially contracted state to support and give solid appearance to the body. When it gets excessively squeezed or strained or gets deprived of oxygen or nutrients, severe muscular contractions may follow, leading to cramps.
All skeletal muscles work voluntarily under our will, but cramps are involuntary, painful,

spasmodic contractions or increased muscle reflex in these skeletal muscles. It may occur during an attempt to move or act quickly or continuing vigorous act without any break or sometimes even at rest or sleep. Children unknowingly jiggle their hands often while writing to get rid of this cramp. Players used to warm up before their game to avoid cramps. Cramp may involve single muscle or a group of muscles. It can also occur in smooth muscles i.e. intestines, in that case it will be called colicky pain rather than a cramp.
Reason for cramp nature of muscle – Cramp pain is the factor which warns us about strain or stretch of the muscle. It also denotes that the affected muscle is out of reach with oxygen or it is loaded with waste products i.e. lactic acid or pyruvic acid. Cramps can also be considered as anti-tear phenomena.
 Incidences
Incidences – Everyone would have experienced cramp in some part of the body muscle at one time or the other. Most commonly, it is experienced in the calf muscle, thigh, hip, hand, neck, etc. Even though it can occur in anyone, it is most commonly experienced by children, players, females, pregnant women and the elderly, when they strain. Also, its incidences seem to be higher, particularly at night, after strained day work or activity.
Causes – In most cases, the cause for cramps cannot been identified. Also muscle cramps have a variety of causative factors, i.e., it may be due to Physiological
Fatigue of Muscle caused by Low nutrition – vitamins or mineral deficiency
Low nutrition – vitamins or mineral deficiency- Strain or strenuous exertion or exercises or games (especially football, tennis, etc.) – here overloading of waste products also accounts for fatigue and muscle cramp
- Sitting idle for a long time in improper posture where blood vessels get compressed. Here muscle gets low oxygen with reduced blood supply in case of compression of blood vessels.
- Dehydration from diarrhoea, fever or any other diseases or even with overdose of diuretics
- Exposure to extremes of temperature
- High altitudes where there is low oxygen supply
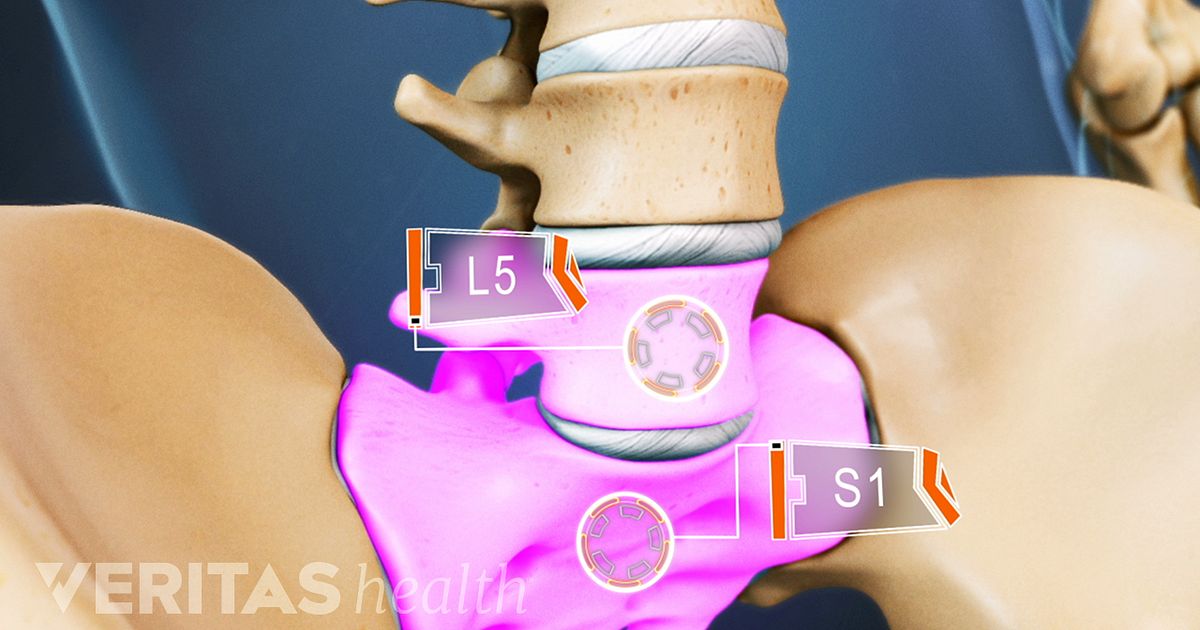
Pregnancy – Here the uterus compresses adjacent blood vessels during first and last trimester of pregnancy where a major part of the pelvis room will be occupied by the enlarging uterus (in first trimester) or descending foetus (third trimester)Excessive sexual activity – Here major part of blood will be naturally deviated to reproductive organs to deprive legs from oxygenated blood.
 Pathological
Pathological- Nervous disorders
- Muscular disorders
- Vascular disorders
- Hormonal disorders especially of thyroid and diabetes
- Auto immune disorders
Habits of - Excessive intake of coffee
- Excessive intake of drinks
- Excessive smoking
Symptoms – There will be two main symptoms i.e. pain and contracture (sustained contraction) of the muscles. In addition, weakness and fear of pain will be there for some more time even after complete disappearance of the cramp. It may come in flashes and go in flashes within seconds. Sometimes, it may be present violently up to 10-15 minutes. It also varies in intensity according the nature of muscles, its nutrition, training and straining, i.e. slightest or painless eye twitch to aggressive painful contracture.
Diagnosis – Most of time, there won’t be any requirement for investigation. But, if cramps recur often, then it is better to evaluate the complaint with the following tests, i.e.
Plain X-rayBlood test – Tc, Dc, Esr, haemoglobin level, sugar, cholesterol, urea, serum calcium, serum potassium, serum magnesium, etc. In children, if one is not sure about the pain to which it is related i.e. either bone or muscles, then it is better to evaluate ASO titre also to rule out rheumatic fever.
Hormones test – thyroid hormones, i.e. T3, T4, TSH
Urine – sugar, albumin and deposits
Finally, if required, one should evaluate with nerve conduction test to rule out nervous disorders, Electromyography to rule out muscular disorders and whole body MRI scan to rule out any other pathology.
Complication – Mostly, there won’t be any complication at all. But recurrent cramps at night may make sufferer sleepless and depressed. Cramps neither remain a serious illness nor let the person free from the fear of having it again. It may also become a hurdle to undertake /do hard work.
PreventionTake
- Plenty of water with glucose or juices
- Plenty of vegetables, nuts and dry fruits
- A break when you happen to walk/ work / travel continuously
- Rest with legs elevated if there is any swelling or oedema
- Treatment for vascular disorders or varicose veins, if any
Do Go for a walk before going to bed
Go for a walk before going to bed- Jog or shake the part involved to get quick circulation
- Warm up of muscles before straining them
- Stretch or massage the muscles involved
- Regular exercise (mainly stretching type)
- Keep legs warm by covering it with blanket while sleeping
- Wear socks / shoes / stockings in cold climate
Avoid- Unnecessary medications
- Standing in water or walking or swimming for a prolonged time
- Tight under garments and tight-fitting socks and shoes
- Smoking, drinking and drugs
General treatment – As everyone knows, cramps never complicates, so no one goes for treatment: they just shake away or kick away or massage the part, i.e. most of the time, treatment is neglected. However, if it happens to recur often and upsets normal activities, treatment should be sought. Also, with treatment, only in the case of severe pain, pain-killers are prescribed after ruling out other diseases. Most of the time, supplements (vitamins and minerals) are prescribed with analgesic ointments to ease the pain.
 Homeopathic approach
Homeopathic approach – People treat cramps in their own way i.e. some with application of warmth, some with external oil, some with external pain balms or analgesics and some even apply turpentine / kerosene / camphor oil, etc. to sooth / ease the muscle cramp and pain. These measures will not relieve the cramps wholly as such, but just mask the suffering for the time being like a pain-killer, i.e. everything needs to be repeated as routine schedule whenever it arises. This is common to all external therapy with respect to cramps. Also using them continuously or often will make it to become useless in the near future.
Repeated abnormal contraction i.e. cramps, can be rooted out easily with internal Homeopathic medicines. Homeopathy medicines increase blood supply to the muscles, increase stamina and the withstanding capacity of the muscles to tolerate any strain. Instead, just providing a pain-killer for the cramp will help only for that day. Homeopathy can ease discomfort and pain of the cramps amazingly without any recurrences by clearing all possible causes.
Homeopathic medicines commonly used in case of cramps are Acid Benz, Actea racemosa, Arg met, Arnica, Belladonna, Bryonia, Calc carb, Calc phos, Causticum, Colocynth, Cuprum met, Ferrum met, Ferrum picricum, Gelsemium, Kali phos, Kalmia, Lachesis, Ledum, Lycopodium, Mag phos, Nat phos, Petroleum, Pulsatilla, Rhus tox, Secale cor, Zinc met, Zinc phos, etc. These Medicines should be taken under the advice and diagnosis of a qualified Homeopath.
for new hope
Dr. S. Chidambaranathan, BHMS, MD (Homeo)
Laxmi Homeo Clinic
24 E. New Mahalipatti Road
Madurai, TN 625 001
India
Tel: +91-452-233-8833 | +91-984-319-1011 (Mob)
Fax: +91-452-233-0196
E-mail: drcheena@yahoo.com
www.drcheena.com / www.drcheena.in
(Disclaimer: The contents of this column are for informational purpose only. The content is not intended to be a substitute for professional healthcare advice, diagnosis, or treatment. Always seek the advice of healthcare professional for any health problem or medical condition.)












 I've had this on my to-do list for probably two years and I can't believe it took me that long. I first learned this from one my favorite herbalists/teachers, Tina Marie Wilcox, who i have mentioned previous.
I've had this on my to-do list for probably two years and I can't believe it took me that long. I first learned this from one my favorite herbalists/teachers, Tina Marie Wilcox, who i have mentioned previous.



 Bleeding Heart. Truly one of the most moving and vulnerable looking flowers in the whole plant Queendom.
Bleeding Heart. Truly one of the most moving and vulnerable looking flowers in the whole plant Queendom.
